Over the past decade, private practice in healthcare has been rapidly declining. Between 2012 to 2022, the share of physicians working in private practice dropped from 60% to 46%. Among younger physicians, over 70% are now employed outside of private practice, mostly larger healthcare systems or private equity owned firms. The reason for the decline is the intimidating challenges facing private practices, notably the financial burden on doctors coming out of medical school, the outsized power of insurers to pay lower rates, and the difficulties of managing administrative and regulatory requirements. It’s simple, right now private equity owned practices and larger hospital systems are the lower risk option for a newly minted doctor coming out of medical school. Let’s dive into why that is deeply concerning.
The Impact on Patients
The implications of healthcare consolidation are drastic. Health care prices due to provider consolidation are estimated to rise anywhere from 3% to 65%. Consolidation can also result in worse care for patients, where large systems are more likely to shut down services in rural communities and providers often overlook preventative care in exchange for higher-margin emergency care because of misaligned incentives between patients and financially-motivated providers. Patients have mistrust of the system because surprise bills appear with seemingly implausible costs. Ultimately, this creates a devastating spiral. Poor health can lead to increased medical expenses, reduced earning capacity, and overall eroding of financial wellness. Financial difficulties mean patients can’t pay for preventative care and necessary treatments, which ultimately lead to worse long-term physical and mental health. As a result, compared to peer nations, life expectancy in the U.S. is lower, hospital admission rates for chronic conditions are higher, and healthcare cost per capita is double. And with larger systems becoming less personalized to the patient, trust becomes even harder to come by and doctors who entered the industry for missionary reasons are frustrated.
However, since 2022 the share of physicians in private practice has stabilized. I believe strong tailwinds are poised to make the next decade look vastly different than the previous one. It’s now time to save private practice.
That’s crazy, why should we believe anything will change?
Let’s break down the three largest barriers to working in private practice and why I believe technological and regulatory tailwinds will help buck the trend.
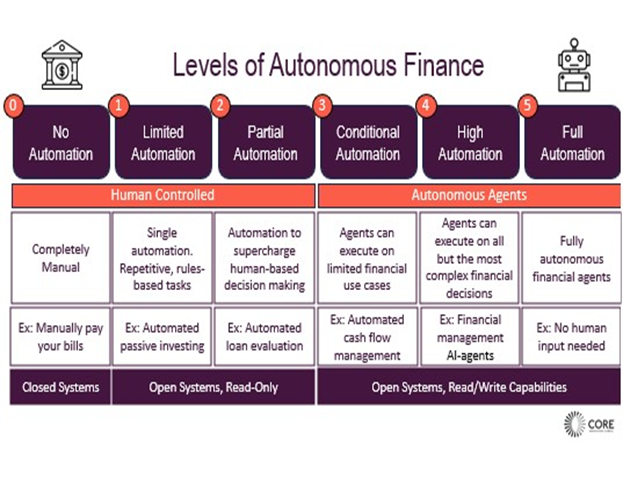
The outsized power of insurers to pay lower rates will decrease in relevance. While the power of incumbents will be entrenched for some time, I see some positive signals of change. First, data is becoming less and less siloed. The Hospital Price Transparency Rule, in effect as of 2021, requires hospitals to publish their prices. As of 2022, the Transparency in Coverage rules requires health insurance plans and issuers to disclose negotiated rates for all services and items. This is the largest collection of healthcare cost data ever published. The 21st Century Cures Act, in effect as of 2022, forces Electronic Medical Record systems (EMRs) and providers to be more open with healthcare data. All in all, we are seeing a system move from closed to open data, similar to a trend that opened the door for a wave of innovation in financial services. Albeit, with low compliance and with unfriendly data formats. Still, as transparency increases, pressure on higher prices and usury practices will increase. Fortuitously, this opening of data happens to coincide with a technological tailwind, deep learning, that makes it easier for small teams to process large, complicated data sets. Power dynamics will begin to moderate.
Second, organizations that empower doctors without taking over their practice are growing in size and capabilities. California, for example, has Independent Physician Associations (IPAs) that are formed to negotiate on behalf of smaller practices and reduce the overall burden on these practices. One physician told me that before working with an IPA, it felt that “we’ve created a system where everyone can make money on a practice, except for the physician themselves.” But after working with the IPA, not only did it lead to better prices, it also led to shared best practices and better care coordination. The IPA represented what felt like the only alternative to selling to private equity. Within Medicare, Accountable Care Organizations (ACOs) are tied to value-based care models. ACOs offer increased bargaining power and shared savings models. With more regulatory push towards quality-based care models and more tech companies helping facilitate these models, we’ll find that payers and providers can actually align on better outcomes. Let’s continue to build tech companies that find ways to increase the bargaining power of small businesses.
Financial burden on practices is a clear problem, but solutions are underway. There is no beating around the bush here, taking ownership of a private practice comes with higher financial risk and operational cost, but ultimately higher reward. There are a few ways in which I see the financial burden ameliorated. First, negotiating reimbursement rates with insurers and high back-office costs mentioned above are part of what drives a challenging business model for private practices. Once again, IPAs, ACOs, and MSOs will alleviate the pain for doctors and AI-driven products will drive these costs down.
Second, Government scrutiny of antitrust dynamics is putting pressure on private equity rollups creating a drop of 65% in roll-up transactions over the past four years. This will become less and less of an option for the majority of practices. Yet, that doesn’t change the fact that there are a growing number of retiring doctors, with 45% aged 55 or older. Instead, selling to the next generation of doctors will become a valued option and seller-based financing, where the doctor sells the practice overtime partially paid for by the profits of the business, will become more prevalent. This ensures that the previous generation shares the financial risk with the next one.
Third, There is an increasing willingness of patients to pay for a subscription when they know they are getting a better service. Membership fees are expected to grow 10% annually over the next decade. I expect more focus on value-based care and PMPM models, giving doctors a more predictable revenue stream.
And lastly, CFO-tooling has been a major theme for fintech over the last few years. Companies building financial operating systems for practices are growing in interest. There’s been more of an emphasis on cash flow management, from startups helping factor insurance receivables to businesses helping practices optimize supply chain management. While doctors are loath to adopt more platforms, I expect these businesses to embed themselves overtime into the workflow of back office administrators and ultimately provide more financial clarity.
Administrative challenges on doctors will be solved by tech. While doctors today spend >50% of their costs and time on administration, over the next decade that will change. Vinod Khosla’s quote that AI will take “80% of 80% of today’s jobs” rings particularly true in this setting. Administrative burdens in healthcare are due to high complexity, large and disparate data systems, loads of unstructured data, an abundance of middlemen, and, of course, high regulatory scrutiny. This is where with the right team knowledge, data sets, and guardrails, a new AI-first system can thrive and ultimately outperform a human-first administrative approach. The companies I’m most excited about in healthcare are taking unique insights, disparate data sets, and modern technology to automate painful workflows in the provider back-office and make starting a business easier. Let’s see the “Stripe Atlas for healthcare.”
At Core, we support the little guy, particularly when there are tailwinds that will force the adoption of technology over the next decade. This is a prime example that, ultimately, will enhance end patients’ health and financial wellness. If you’re building to empower private practices and quality-based care models, we’d love to speak with you. Particularly if you are using AI to force systemic change.